President Trump’s nominee for surgeon general, Dr. Casey Means, is a prominent proponent of continuous glucose monitoring.
(It measures the sugar concentration between your skin cells, which roughly correlates with your blood sugar level.)
The quick feedback from a continuous glucose monitor may give them a nudge to actually implement nutritional advice.
Another small study, in the same journal, found that the continuous glucose monitor overestimated people’s blood sugar levels compared with directly measuring it in the blood.
Third, some people can have what looks like normal blood sugar levels but still have insulin resistance, Kennedy explains.
Even though the gadget is tiny, there is a lot of excitement surrounding it.
Despite being only slightly larger than a quarter, the companies that sell continuous glucose monitors make extravagant claims about their health benefits: One company claims that you can “revolutionize your health.”.
One of the leading proponents of continuous glucose monitoring is Dr. Casey Means, President Trump’s choice for surgeon general. She is one of the founders of a company that sells an app to assist users and distributes the devices.
A painless patch that adheres to your skin is the monitor. It provides an estimate of your blood sugar to a phone app every few minutes or so. It gauges the amount of sugar present in the spaces between your skin cells, which is approximately equivalent to your blood sugar level. In order to monitor the effects of various foods on your blood sugar, the app also assists you in keeping a food journal.
Research indicates that this technology has revolutionized the way individuals with diabetes are cared for. “It has completely changed their lives and the lives of their families,” says Elizabeth Selvin, a diabetes researcher at Johns Hopkins University.
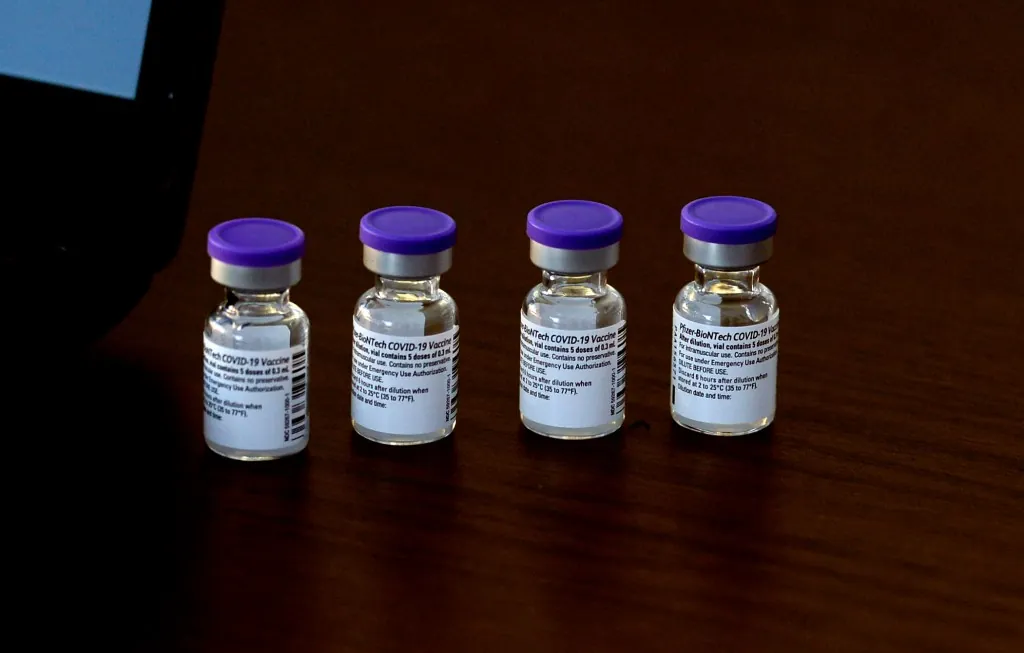
The first continuous glucose monitors for non-diabetics were approved by the Food and Drug Administration in March 2024. They are currently produced by Abbott and Dexcom. Since each patch costs about $50 and lasts for two weeks, monitoring your blood sugar for a long time will cost you about $100 a month.
The crucial query is whether they genuinely aid in the health improvement of those who do not have diabetes or prediabetes.
the hypothesis.
The blood sugar of a healthy individual rises, peaks, and then gradually returns to baseline after consuming a carbohydrate-containing meal.
“These peaks and troughs are the normal physiological response to consuming carbohydrates, in people without diabetes,” says Sarah Berry, a nutritionist and King’s College London nutrition professor. In addition, Berry serves as chief scientist for Zoe, a business that sells continuous glucose monitors (CGMs) and an app for data interpretation. “We do not need to flatten these curves,” she asserts.
However, Berry notes that when these peaks become excessively high and frequent, issues may occur. According to studies, doing so may increase your risk of obesity, cancer, heart disease, and Type 2 diabetes. Berry adds that it can increase your appetite in between meals, which will lead to a larger meal at the next meal.
The concept behind glucose monitoring is that it may be able to assist you in determining which meals or portion sizes result in the most extreme peaks. This change could then help you lose weight, lower your risk of developing diabetes, or just feel better overall.
conclusions.
This theory has been tested in two large studies using randomized control trials. During the studies, participants tracked their food intake using an app while wearing a glucose monitoring patch for a while. A customized diet plan aimed at reducing blood sugar was created by researchers using the data. The researchers then evaluated the CGM-based diet’s performance in comparison to a typical low-fat or Mediterranean diet.
Mixed results have been found at the population level. A study conducted at the Weizmann Institute of Science found that merely adhering to the Mediterranean diet was more effective in promoting weight loss than the CGM-based diet. Scientists noted in the journal Diabetes Care that it did, however, assist them in lowering their blood sugar levels more.
The second study contrasted a low-fat, high-whole-grain diet with the CGM-based diet. In the American Journal of Clinical Nutrition and JAMA Network Open, researchers from New York University found that both diets produced modest improvements in blood sugar and about the same amount of weight loss on average. However, the study’s overall results don’t fully tell the story, according to Collin Popp, who assisted in leading it. According to Popp, these findings only reflect the typical response from the entire population.
“It’s very different when you look at the individual level,” he says. The glucose-monitoring method was very beneficial for some people. A significant amount of weight was lost by some people. “People returned to tell us, ‘You changed my life.'”. I feel fantastic now that I’ve shed thirty pounds. Other study participants gained weight. “..”.
Currently, researchers are attempting to determine who stands to gain from this technology.
When do glucose monitors come in handy?
1. . if your sensitivity to carbohydrates is very high.
For the past five years, nutritionist Karen Kennedy has been assisting individuals in deciphering and comprehending their glucose-monitoring data. She has found that some people use these devices to identify a heightened sensitivity to carbohydrates, even those that are healthy, like whole grains.
“When they consume brown rice, quinoa, beans, rice, or oatmeal, their blood glucose levels regularly rise,” she says.
They come to understand that a low-carb diet will help them better control their blood sugar levels thanks to the monitor. Kennedy states that “there should be fewer carbohydrates, not zero.”.
Kennedy states that “they drastically lower their blood sugar after making dietary changes.”. “They feel better and reduce visceral fat if they can stick to the new diet. “..”.
2. if you require additional encouragement to consume more healthful foods.
The steps that people need to take to improve their metabolic health are already well known. It’s difficult to put this advice into practice, according to Kennedy and Popp of NYU.
A continuous glucose monitor’s prompt feedback could encourage them to follow dietary recommendations. “It’s a motivator,” replies Popp.
Kennedy, for instance, knew that one of his clients needed to increase the amount of fat and protein in their breakfast.
“I’m sorry, but this has been my breakfast for thirty years,” they said. ‘”.
After wearing the patch for a week, the client noticed that breakfast caused their blood sugar to spike. Kennedy claims that they promptly altered their breakfast. The customer immediately noticed an improvement in their blood sugar levels after trying this new breakfast.
She claims that “they didn’t have to wait a few months and visit the doctor to see it working.”. “That autonomy can serve as inspiration. “.”.
3. . if you need to be more mindful of your diet.
Some of the participants in the NYU study benefited significantly from the CGM-based diet. Upon further examining their data, Popp and his colleague discovered a crucial element that contributed to this success: whether or not the participant regularly entered their mealtimes into the device’s app during the six-month trial.
According to Popp, some individuals found that just keeping a food journal improved their blood sugar levels and diet. “I frequently advise people that keeping a close eye on their behavior can have a significant impact on their health. “.”.
Additionally, he says, “You don’t have to accurately log the food.”. For most people, the act of documenting it is what matters most. “.”.
“We know that awareness helps people lose weight,” Selvin of Johns Hopkins continues. Additionally, an app is not required. One of my coworkers makes use of a small pocket notepad. It’s less expensive than glucose monitoring and adds accountability.
Experts advise being aware of the following before purchasing the device.
The data is confusing and useless to many people.
I get a lot of people who say, ‘I have all this data and I have been using the device for three or even twelve months, but I don’t know what it means. Kennedy states, “I have no idea how to improve or lower my blood sugar.”.
Popp concurs that people truly need to be informed about the significance of the data. However, since scientists and physicians are still baffled by some of the data, that education will only go so far.
The meaning of the peaks and troughs is still unknown to scientists if you’re staying within a normal range, say between 70 and 140 mg/dL.
Popp asserts that there are no clear-cut rules regarding what constitutes a good or bad peak in people without diabetes.
The information may be deceptive.
First of all, our bodies frequently react differently to different foods, and the devices aren’t very accurate or precise. The same meal consumed on two different days produced wildly disparate readings, according to a recent study published in The American Journal of Clinical Nutrition. In contrast to measuring blood sugar levels directly, a different small study published in the same journal discovered that continuous glucose monitors overestimated people’s blood sugar levels.
Second, the information may cause people to stop eating nutritious foods that cause normal blood sugar fluctuations or to worry about doing so. Popp’s friend, for instance, became concerned about blueberries after they caused her blood sugar to slightly increase before falling.
Foods shouldn’t be labeled as “unhealthy” just because they caused what I thought was a very slight rise in blood sugar. “.
Third, according to Kennedy, some people may have insulin resistance even though their blood sugar levels appear to be normal. Their bodies overproduce insulin in this situation as a compensatory mechanism. You would need to visit a doctor and have your insulin levels measured in order to determine this.
“A useful metric is continuous glucose,” she says. However, it’s only one metric, and you must use it in conjunction with other symptoms and lab results. “.”.
With Jane Greenhalgh as editor.